The Lived Experience of Fatigue and Post-Exertional Malaise: Part 1
Jun 14, 2025
How are they similar, and how are they different?
Welcome to a four-part blog series on one of the most important topics in our community: fatigue and post-exertional malaise. I frequently receive emails asking about these two core symptoms, how they differ, and who is affected by them. This blog sets out to answer these questions.
In Part 1, I describe what it feels like to experience fatigue and post-exertional malaise (PEM). As you read that section, consider which of these symptoms you identify with most.
In Part 2, I share some research findings that validate that fatigue and PEM are real and that they are different.
In Part 3, I summarize some leading ideas about what causes PEM.
In Part 4, I discuss some emerging treatments for fatigue and PEM. Since the underlying biology of fatigue and PEM differs, effective management also varies.
What Is Fatigue?
Fatigue means different things to different people. Most people think of fatigue as a sense of tiredness or lack of energy that interferes with their usual daily activities. The bottom line is that people with fatigue have less capacity to do the things they used to be able to do before the fatigue started.
Here are some descriptions of fatigue from participants at a recent live discussion I had with members of the Fibromyalgia Support Network. Note how diverse these experiences are:
- drained of energy, weak, nothing left in the battery
- trouble concentrating and remembering
- feels like I'm wearing a lead blanket or cloak
- it is like I have been drugged
- limbs feel super heavy—it’s hard to walk
- so much effort is required for everything
- exhausted, hard to hold eyes open
- decisions are impossible
- can't deal emotionally with any unexpected or urgent events
- body pain is high
- fatigue that mimics stroke-like symptoms, head is heavy, mouth is like cotton balls
- hard to move your body
Fatigue is very common. A recent meta-analysis (a study combining the results of many other studies) reports that 20% of adults and 10% of minors under the age of 18 experience fatigue severe enough to interfere with normal activities (Yoon et al., 2023).
- Fatigue is more common in women than men, a finding that is in desperate need of research so we can understand why.
- Unexplained fatigue is more common than fatigue due to a known medical condition. This means that most people with fatigue don’t know why.
Fatigue is not a disease. It is a symptom associated with a huge list of underlying problems. The first step in solving fatigue is to look for, identify and remedy the underlying causes.
In the general population, fatigue can be related to
- doing too much in our busy, modern lifestyle.
- tiredness or sleepiness due to poor sleep quality or insufficient duration.
- mental health problems such as anxiety and depression.
- a diet low in essential nutrients, irregular eating patterns, or excessive sugar and processed food.
- a sedentary, modern lifestyle lacking the necessary stresses our body needs to be healthy and able to function.
- medical conditions like anemia, hypothyroidism, diabetes, sleep apnea, and cancer.
- some drugs, including many cancer treatments (cancer-related fatigue).
The fatigue experienced by people with myalgic encephalomyelitis, chronic fatigue syndrome, long COVID and possibly fibromyalgia has some specific characteristics not reported by healthy people.
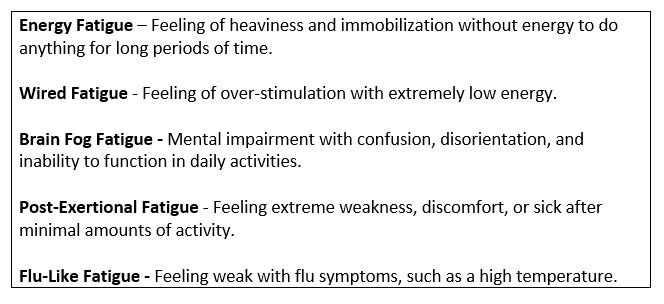
Leonard Jason and colleagues identified five fatigue types that are common in ME/CFS and FM but not in the general population (Jason et al., 2010). In my clinical experience, virtually all people with ME, long COVID and FM experience the fatigue types described in the chart below. Healthy people only experience flu-like fatigue, and then, only when they actually have the flu, not as a daily experience.
Fatigue Types Experienced in ME/CFS
From Jason and Colleagues
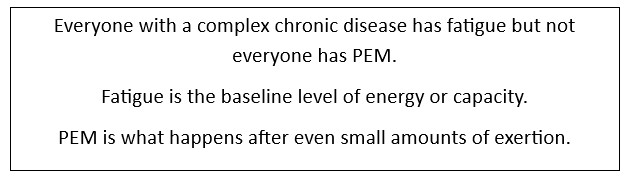
If you have post-exertional malaise, it’s a different ball game.
What Is Post-Exertional Malaise?
- Post-exertional malaise (PEM) is the hallmark symptom of long COVID, myalgic encephalomyelitis and chronic fatigue syndrome.
- PEM involves worsening of fatigue and other symptoms after relatively minor mental, physical or social exertion.
- The worsening usually begins within 3 days of the exertion and by definition lasts more than 24 hours.
- People who are more severely ill generally have worse PEM. They crash more easily, sooner and harder and take longer to recover.
- PEM is a major cause of disability in people with ME and long COVID, so understanding the biology of PEM and potentially how to lessen it is of great importance.
What Does Post-Exertional Malaise Feel Like?
Here are some examples from participants from the recent Fibromyalgia Support Network event. After an activity, the intensity of which is different for everyone, people with PEM may have experiences like the following:
- After a yoga class, not only can I not do yoga the next day, but I also have a crash right after, which is like narcolepsy; I need to sleep, and I cannot stop it.
- It’s like hitting a wall, getting hit with a bad flu and cold at the same time, like every nerve ending jangling, and/or whole-body throbbing.
- PEM is the total inability to be dependable.
- It is the inability to know how emotions, stress, movement, etc., will affect me or my ability to function.
- It is feeling weighed down with pain and fatigue.
- I get brain fog, can't handle stimulation, trouble finding words, and feel irritable.
- Any exercise out of the ordinary (like a longer walk, a bit of gardening, extra loads of laundry) will mean I am deeply fatigued and not up to anything the next day.
Take Home Message
From an experiential perspective, fatigue and PEM are different. In Part 2, I ask whether this is reflected in measurable tests.
To see the Video Tip corresponding to this blog, click here.
If you liked this blog, you may also like the following similar blogs:
https://www.eleanorsteinmd.ca/blog/fatigue-part-4
https://www.eleanorsteinmd.ca/blog/fatigue-part-3
https://www.eleanorsteinmd.ca/blog/fatigue-part-2
https://www.eleanorsteinmd.ca/blog/Mitodicure
To learn more about Pathways to Improvement, click on the image below!
References
Jason, L. A., Boulton, A., Porter, N. S., Jessen, T., Njoku, M. G., & Friedberg, F. (2010). Classification of myalgic encephalomyelitis/chronic fatigue syndrome by types of fatigue. Behav. Med, 36(1), 24–31. doi:10.1080/08964280903521370
Yoon, J. H., Park, N. H., Kang, Y. E., Ahn, Y. C., Lee, E. J., & Son, C. G. (2023). The demographic features of fatigue in the general population worldwide: a systematic review and meta-analysis. Front Public Health, 11, 1192121. doi:10.3389/fpubh.2023.1192121