Fatigue and Post-Exertional Malaise Part 4
Jul 07, 2025
Emerging Science-Based Management of Fatigue and Post-Exertional Malaise
In the final part of this in-depth analysis of fatigue and post-exertional malaise (PEM), I focus on management. I wish I had more evidence-based (aka research-proven) strategies to share. I have been going to international ME/CFS meetings since 2000. Every year, I attend with optimism, hoping to hear something definitive that I can pass along.
So far, self-management remains the best approach. It is not evidence-based, but it has 40 years of empirical support, meaning that when people are aware of what makes them feel worse and better and listen to their bodies, they do better.
I start this blog post with one of the most controversial topics in our field, discussing whether and when activity treatment can be useful and when it is less so. Then I introduce some newer treatments that are currently being researched.
1. Can Movement Be Therapeutic?
One of the most common questions I am asked is how to decrease fatigue and PEM so that people can return to the activities they love. Most people with ME, CFS, FM and long COVID have had repeated failures attempting to increase their activity levels. They push through and then crash. When this occurs repeatedly, we call it the “push/crash cycle.”
We hear all around us that activity is healthy, so when it doesn’t work for people, they are left wondering what is wrong with them that they can’t improve their stamina.
Here's the dilemma. We only get stronger and more resilient if we challenge our bodies. In healthy individuals, muscles become stronger and more resilient in response to activity. And muscles that are not exercised lose capacity.
The challenge for people with fatigue and PEM is to find ways of moving that will encourage these gains without causing a crash. This means doing the right type of movement, in the right dose, and on the right schedule for each individual. This appears to be an area where fatigue and PEM are different. For example, as a group, people with FM (who, according to dogma, have fatigue but not PEM) benefit from mild to moderate aerobic and strength activities, whereas people with PEM do not.
Activity Management in Fibromyalgia
- A 2017 Canadian review of studies of aerobic exercise treatment in FM shows that compared to individuals with FM who aren’t exercising, those who do regular aerobic exercise show small improvements in quality of life, pain, stiffness, physical function, and fatigue.
- For FM, aerobic activity is slightly better than strength training in terms of symptom benefit.
Some Caveats
- Longer-term follow-up shows that only physical function and pain remain improved for more than six months after stopping supervised exercise (Bidonde et al., 2017).
- The improvements ranged from 6–11% compared to those who didn’t exercise. This is a very small improvement.
- Participants in research studies were taught how to exercise safely, and their progress was monitored at regular intervals. Ordinary patients told to “exercise” by their family physicians and given no further guidance are unlikely to do as well as those in the research studies.
- Exercise prescriptions need to be tailored to individuals, taking into account what activities they enjoy, their capacity for activity and the degree of post-exertional malaise they experience.
- The trick is finding what you like doing. If you don’t enjoy the activity, you are unlikely to do it over the long term.
- You don’t have to attend a class. You don’t have to leave your home. For some individuals, a personalized program of increased movement during ordinary activities will be more enticing and productive than intentional exercise.
Post-Exertional Malaise Is Different from Fatigue
If you experience PEM, the goal is NOT to increase your activity level but rather to avoid PEM crashes.
- It is becoming clear that to recover and heal from PEM, it is necessary to avoid crashing too hard or too often.
- How does one avoid crashing? Through PACING (Casson et al., 2023).
- Careful pacing for PEM means limiting your activities so that you stay within your energy envelope (Jason, Muldowney, & Torres-Harding, 2008). This means ensuring you can recover to your baseline within 24 hours.
- For people who are severely ill, staying within one’s energy envelope can be difficult or impossible. Avoiding PEM crashes is easier said than done. For most, it is an aspiration that is not always possible.
- To help people with this goal, I have developed a strategy called DEEP pacing. DEEP pacing involves carefully monitoring your mind/body for early warning signals of an impending crash and overcoming your beliefs that get in the way of effective pacing. You know those pesky beliefs that you are being lazy and should push through?
- To help you implement DEEP pacing and DEEP self-care, I have created recordings of two webinars. It is key to be gentle with yourself and take baby steps towards healing rather than giant leaps, only to trigger a setback.
Other Possible (i.e., not yet proven) Management Tools for Post-Exertional Malaise
2. Mitochondrial Support
Many people reason that if the mitochondria are not producing enough energy, perhaps it is because they don’t have access to some of the molecules they need to function optimally. This is the rationale behind something called “mitochondrial protocols,” typically a cocktail of supplements to support the mitochondria in switching from glycolysis to oxidative phosphorylation and produce more energy.
In my experience, a minority of patients benefit from this approach. I’ve never observed the success that other practitioners claim. The most likely explanation is that the mitochondria in non-responders are stuck in the cell danger response in ways that are not addressed by the supplements. If the mitochondria have geared down as a protective strategy, it is unlikely that supplements will change this unless the underlying cause is shifted. Even if modestly effective, mitochondrial protocols are expensive and hard to maintain over the long term.
An example of a popular mitochondrial protocol is that of Dr. Sarah Myhill. It includes supplements such as Coenzyme Q10, NADH, magnesium, fish oil, L-carnitine, vitamin D and more.
3. Therapies to Balance the Immune System
If PEM is related to inflammation, it stands to reason that anti-inflammatory drugs should help. However, this has not been effective in preliminary studies. Researchers are looking for other strategies to calm and balance the immune system.
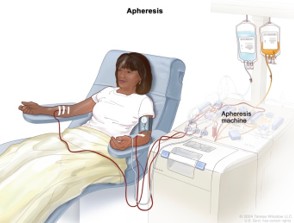
Strategies like immunoadsorption therapy, which filters the blood to remove autoantibodies and fibrin clots, are being researched at Charité hospital in Berlin with some modestly supportive findings. Controlled research is necessary to identify who may benefit and ensure that treatment is safe (Tölle et al., 2020).
Intravenous immune globulin injections (IVIG) are being researched again after a 30-year hiatus. A recent study of IVIG in long COVID patients with neurological symptoms showed a positive response. Two large-scale studies are currently underway for long COVID, including the RECOVER study, which I have previously written about.
A couple of cautionary notes. The benefits of IVIG wear off within about 3 months of ending treatment, meaning this is not a cure but rather a palliative measure. IVIG treatment is very expensive and not widely accessible. Even if the research underway shows benefits, the average patient with ME or long COVID will be unable to access it.
4. Treatments to Improve Blood Flow and Oxygen Absorption
In theory, hyperbaric oxygen therapy (breathing 100% O2 under pressure) should improve blood flow and oxygen extraction by tissues. The increased oxygen level in the blood and tissues improves mitochondrial function, which enables the tiny blood vessels and the cells that line them to deliver blood to where it is needed. Studies have shown improvement in patients with long COVID for symptoms including overall quality of life, sleep quality, pain and cognitive function (Hadanny et al., 2024; Wu et al., 2024).
Anticoagulant therapies have been studied to address microclot formation. A recent meta-analysis suggests that anticoagulant therapies reduce the risk of major blood clots and all-cause mortality. Unfortunately, the paper doesn’t comment on whether it improves the quality of life for people with long COVID (Zhou, Yang, Wang, Hou, & Song, 2024).
The Good News—Research Is Advancing
It can be frustrating and disheartening to attend conferences year after year and hear so little clinical research with positive findings. But there is good news.
- Research in the field of ME and long COVID is increasing exponentially, with skilled, interdisciplinary research teams now active in several countries.
- Collaboration between groups is replacing the siloed approach of the past. New researchers are joining the field, bringing their diverse expertise with them. ME and long COVID are now considered legitimate areas of exploration rather than being labelled as “career killers.”
- Many new findings about what is going wrong in PEM are being discovered, including those I discuss in this blogpost.
However, there is often a frustratingly long delay between the discovery of an abnormality and figuring out how to fix it. Things that sound great in theory often fail to translate into gains for real patients in controlled research studies.
With so many systems functioning abnormally, the goal in PEM research is to find something upstream of the abnormalities. That way, fixing one or a small number of processes will have a positive domino effect on everything downstream.
Join Me to Keep Up With New Findings.
Keeping one’s finger on the pulse is hard work. My goal is to save you time and energy by sharing important advances in concise, digestible bites across multiple formats, tailored to your preferred learning style.
I share what I’m learning in real-time through my blog, my video tips of the month, my subscription-based membership, Live! with Dr. Stein, and on my new podcast, The Dr. Eleanor Stein Podcast.
I welcome your feedback on my published blogs and suggestions for topics you'd like to learn more about.