Research Update on Fibromyalgia, 2021
Oct 11, 2021The Third International Virtual Congress on Fibromyalgia
On June 24 - 25 I attended the Third International Virtual Congress on Fibromyalgia. Many of the presenters were from Europe and were people I had not heard before. They discussed many important topics on FM including the lack of a definitive definition, lack of a diagnostic test and lack of effective treatment options. Not too much to report there.
There was one very interesting theme running through the conference - a new understanding of what causes persistent pain disorders including FM. This new understanding is based on extensive research that FM is in large part caused by brain neuroplasticity. This research is now widely accepted, so much so that the International Association for the Study of Pain has created a new pain category called nociplastic pain to include FM and other persistent pain disorders.
This blogpost explains the scientific rationale for this major shift in understanding persistent pain. And I introduce something that wasn’t discussed at the conference - how conditions caused by neuroplasticity can be treated and improved. Read on to learn how to rewire your brain to decrease persistent pain.
What Is Neuroplasticity?
 Neuroplasticity is the change of brain structure and function throughout the lifespan in response to experience. Everything we think, feel and do influences our neuronal connections in real-time. Neuroplasticity helps all animals who have neurons adapt to changes in their circumstances. Neuroplasticity can change brain function for the better or worse. It can cause problems and can help us reverse them.
Neuroplasticity is the change of brain structure and function throughout the lifespan in response to experience. Everything we think, feel and do influences our neuronal connections in real-time. Neuroplasticity helps all animals who have neurons adapt to changes in their circumstances. Neuroplasticity can change brain function for the better or worse. It can cause problems and can help us reverse them.
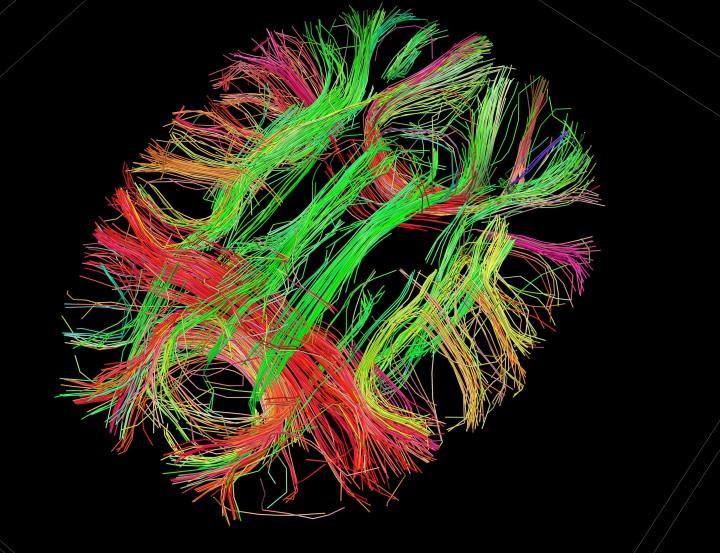
Photo of the human connectome (brain pathways)
There are three main pain types: Nociceptive, Neuropathic and the New Category Nociplastic.
What Is Nociceptive Pain?
Nociceptive pain is what we usually call “acute pain”. It is generally caused by an injury like a broken bone, surgery or inflammation such as that caused by arthritis. Nociceptive or acute pain is sharp, localized to the affected area and feels better with ice. If there is no re-injury, it heals within 8 weeks. Nociceptive pain often responds well to pain killers such as non-steroidal anti-inflammatories which decrease inflammation. If nociceptive pain is not adequately treated the risk of transition to chronic pain increases. This highlights the importance of good post-surgical and injury pain management.
What is Neuropathic Pain?
Neuropathic pain is caused by damage or inflammation of the nerves themselves. The most common examples are the pain in the hands and feet of people with diabetes. The pain from shingles is another example of neuropathic pain. Neuropathic pain is often associated with other neurological signs such as numbness, tingling, changes in temperature and blood flow. It is generally considered very difficult to treat and likely to be chronic. The most common medications used for this type of pain are tricyclic antidepressants such as amitriptyline and drugs like gabapentin. These drugs act on the nervous system to decrease pain transmission.
What Is Nociplastic Pain? (The new pain on the block)
Fibromyalgia (FM) is now officially classified by the International Association for the Study of Pain as a nociplastic primary pain disorder. The primary cause of pain in FM is hyperactive pain processing in the brain and spinal cord.
Nociplastic pain has certain characteristics which are different from nociceptive pain and neuropathic pain. In this blog post I use the terms persistent pain and nociplastic pain interchangeably. These characteristics include:
- Pain lingers after the expected time for tissue healing (eight weeks).
- Pain spreads to many areas of the body (“pain all over”).
- Hypersensitivity to touch, temperature and pressure.
- Association with symptoms such as fatigue, unrefreshing sleep, brain fog and hypersensitivity to sound and light.
- Pain feels better with heat.
In a recent review of Fibromyalgia by rheumatology professor Piercarlo Sarzi-Puttini and colleagues, I found the provocative statement that nociplastic pain is caused by “mostly reversible modifications to the nervous system”. This is a huge change in our understanding of persistent pain. For decades, pain sufferers have been told they need to learn to manage or cope with their symptoms because there is no cure. Approved pain medications are woefully inadequate and sometimes cause side effects that are difficult to tolerate. Unfortunately, the authors of recent reviews don’t explain how to modify the nervous system to reverse nociplastic pain.
Nociplastic (Persistent) Pain Is Caused by the Brain
But do not despair. I have been studying and teaching how to reverse the neuroplastic changes that cause nociplastic pain for over 7 years. In the groups I facilitate in my medical practice, I start with the Explain Pain neuroscience education of David Butler and Lorimer Moseley. The first step is to shift from the inaccurate belief that persistent pain is a sign of tissue damage to the accurate belief that it is created when the brain senses danger. Three points should be emphasized here.
- The brain is prone to error when assessing danger.
- The brain builds and strengthens pathways that support its belief whether correct or not.
- All brain pathways can be altered by our choices of thoughts, feelings and behaviours.
In his TEDx talk Why Things Hurt Lorimer Moseley gives several evidence-based examples and one humorous personal anecdote to support this statement. Understanding persistent pain (now called nociplastic pain) is created by the brain imparts short-term reductions in pain and disability. To learn more about the Explain Pain approach, check out the video recording by psychologist Dr. Michelle DeLisle in a 2016 blog post on my website. The question is how to build on this foundation to reverse nociplastic pain.
Is all Chronic Pain Nociplastic?
Pain researchers Lorimer Moseley and David Butler state that 100% of chronic or persistent pain is caused by the brain and not the body. In other words, all chronic pain is nociplastic. People often ask about conditions like arthritis in which pain seems to be caused by recurrent pressure or damage to tissues by osteophytes (bony growths found in osteoarthritis). Butler and Moselely counter with the now extensive evidence that X-ray ratings of arthritis severity correlate very poorly with reported pain levels. In other words, the correlation between objective and subjective findings is weak. This means that some people’s brains have become sensitized to the recurrent physical injuries and others’ have not. So even in the case of apparently recurrent “acute” pain, nociplastic changes are the cause of perceived pain.
Is Nociplastic Pain Reversible?
Fortunately, there are specific strategies to reverse the neuroplastic brain changes that perpetuate increased pain sensitivity. In their manual Neuroplastic Transformation, Michael Moskowitz and Marla Golden explain how to put neuroplasticity into action to reverse persistent pain:
- The brain pathways that process pain also enable other actions such as thinking clearly, moving, feeling, creating and connecting with others.
- Neurons cannot do two things at once. Once they fire, neurons need time to prepare to fire again.
- If the brain is busy creating pain it cannot generate the activities which make life worth living.
- If you busy your brain with engaging, uplifting thoughts, feelings and activities, the brain cannot process pain at the same time.
How Can I Reverse Nociplastic Pain?
Based on this scientific fact, Moskowitz and Golden recommend using each moment of awareness of pain as an opportunity to change one’s thoughts, feelings or behavior to overrides pain processing. What can one do? Anything but thinking about and acting on the pain. They list hundreds of suggestions in their manual and on their free website, Neuroplastix.com. Here are a few examples to give you an idea:
- Try soft touch, warm baths, gentle movement or physical contact with a loved one.
- Exercise decreases both the sensation of pain and the emotional impact of pain.
- Empathy and helping others decrease the perception of pain.
- Imagine the pain processing centers in your brain cooling down (e.g., getting cooler and less fiery). Imagining something associated with positive emotions blocks pain.
- Remind yourself that this persistent pain serves no purpose.
- Use calming scents like peppermint (for those without MCS).
In the 6 years, I have been facilitating groups supporting patients with these strategies, most participants report improvements in pain after the group. For some, these improvements have been long-lasting and life-changing. People have been able to return to activities they love like walking, socializing and working. The first step is becoming open to the evidence that pain is caused by the brain. Once that fact is accepted, participants move ahead with the strategies. Those who commit more time and who choose a variety of active activities to override pain processing do best.
The participants in my Transforming Pain group have mostly had some combination of ME/CFS or FM as their primary diagnosis. They have a wide variety of pain types including FM pain, migraine headache, TMJ, IBS, arthritis and more. My experience supports the research that any nociplastic pain can respond to a neuroplastic approach. There is a need for research to assess this hopeful finding in a controlled manner and to identify which aspects of this approach result in the improvements for what types of nociplastic pain.
It doesn’t matter how long you have been suffering with pain, change is possible. I provide an overview in the Pathways to Improvement course and hope to create a single session Pathway for pain in the near future.
Author: Eleanor (Ellie) Stein MD FRCP(C)
I am a psychiatrist with a small private practice in Calgary and am an assistant clinical professor in the faculty of medicine at the University of Calgary. Since 2000, I have worked with over 1000 patients, all with ME/CFS, FM and ES. My passion for this field comes from my own struggle with these diseases, my desire to improve my health and then pass on what I learn. My goal is for every patient in Canada to have access to respectful, effective health care within the publicly funded system.
Ready to take back your health?
Check out more resources to help combat ME/CFS, FM and ES


