fMRI Evidence - Neuroplastic Intervention Is Effective for Chronic Low Back Pain
Oct 19, 2021Hot off the Press! Research Update
If you have read my blog posts or attended my online course Pathways to Improvment, you will know that I have become increasingly interested in the power of neuroplasticity and other mediators of biological change such as epigenetics and the microbiome to address health symptoms. My interest is in finding strategies that we can do ourselves (self-management) rather than relying on supplements and treatments which may be expensive and have serious side effects. Since ME/CFS, FM and ES are biomedical conditions with measurable abnormalities, legitimate interventions must show measurable biological impact. That evidence is now available. Keep reading to learn more.
Biomedical Research on Neuroplasticity-based Interventions Is Emerging.
A peer reviewed study by Ashar and colleagues has been just been published in JAMA Psychiatry of a new neuroplasticity-based therapy called Pain Reprocessing Therapy. The study results are stunning. In an intent to treat analysis, 66% of participants with chronic back pain who started the treatment reported being pain-free or nearly pain-free after 4 weeks of treatment. And the treatment effects were just as strong one year later. The participants had had back pain for 10.7 years on average. Only 20% of those receiving a placebo injection and 10% of those receiving usual medical care reported a similar improvement. The study included functional MRI assessments before and after the treatment to see whether the brain changed congruent with the participant's subjective reports. (more on this later)
To read more of this open access paper click here
From: Ashar, Y. K., Gordon, A., Schubiner, H., Uipi, C., Knight, K., Anderson, Z., . . . Wager, T. D. (2021). Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain: A Randomized Clinical Trial. JAMA psychiatry.
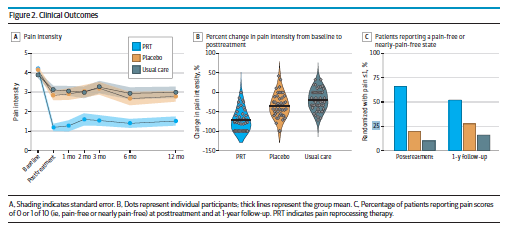
Figure 2 above shows the clinical outcomes from the Ashar paper.
The first image shows differences in pain intensity between the blue (Pain Reprocessing Therapy) and orange (placebo) groups.
The third image shows the number of participants who reported being pain-free after 4 weeks of treatment and at 1 year followup.
It is rare to unheard of in pain research to see such large differences between the treatment and control groups.
What is Pain Reprocessing Therapy?
Pain Reprocessing Therapy consists of 8 individual sessions - twice weekly for 4 weeks and has 5 components.
- Learning that chronic pain is caused by the brain and is therefore reversible. E.g., My pain is not a sign of tissue damage.
- Gathering personalized evidence for this by identifying indicators of centralized pain in the individual such as pain originating without injury and inconsistency in how pain presents.
- Reappraising pain sensations in real time (somatic tracking) through this lens of safety. E.g., I am noticing pain right now. I know it is due to my brain misinterpreting the signals from my body and I am safe.
- Addressing specific emotional threats including those from life circumstances other than pain. Developing self-compassion.
- Gravitating towards and inducing positive feelings and sensations to move from danger mode to safety mode.
The authors describe how Pain Reprocessing Therapy is different from and expands upon existing approaches such as Cognitive Behavior Therapy, Acceptance based therapies, Mindfulness Based Stress Reduction and Neuroscience Pain Education. Based on secondary analyses from the study, they believe the essential components are:
- Helping participants gain personal knowledge that their pain is caused by the brain.
- Reappraising pain as reversible rather than due to tissue damage.
- Combining cognitive, reappraisal and exposure based components.
What Did the Functional MRI Results Show?
You may be wondering ... what about the objective measures? In this study all participants had a functional MRI (fMRI) before starting the Pain Reprocessing Therapy and again 4 weeks later, after they had completed the 8 individual coaching sessions. While in the MRI scanner they were asked to trigger back pain with a series of specific movements to distend the back at four intensity levels and to rate their spontaneous pain once per minute.
Compared with placebo injection and treatment as usual, Pain Reprocessing Therapy reduced pain-related brain activity in areas related to the detection and inhibition of pain (prefrontal cortex, cingulate cortex and insula). This suggests that after 4 weeks of treatment, the brain was less preoccupied with pain.
From: Ashar, Y. K., Gordon, A., Schubiner, H., Uipi, C., Knight, K., Anderson, Z., . . . Wager, T. D. (2021). Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain: A Randomized Clinical Trial. JAMA psychiatry.
Figure E. above shows that Pain Reprocessing Therapy increased connectivity between the prefrontal cortex (red in the above figure), the insula (green) and the sensory area of the brain. The prefrontal cortex and insula are brain areas that balance the limbic system (the threat detection center). These objective measures show changes in brain structure and function (neuroplasticity) in areas known to be relevant to pain.
Study Limitations
A few limitations should be noted. This is a small study of 151 participants. The results need to be replicated by other research teams to ensure they are valid. The participants in this study had low back pain and not FM or ME/CFS. Research suggests the neuroplastic processes are similar in all types of persistent pain. Never the less, it will be important to see if people with FM will respond similarly. The pain levels of the participants in this study were mild to moderate averaging 4.2/10. Most of FM patients have much higher pain levels and will want to know whether this approach can work for them.
Is This Study Legitimate?
Does this study pass the sniff test? Does it fit with what patients report when they use neuroplasticity-based strategies? In the groups I facilitate in my medical practice for people with persistent pain of all types and severity, the results are similar. The majority of people, including those with FM report improvement. Duration and severity of pain do not seem to be a limiting factor. Even people who have experienced severe, daily pain for decades have substantially recovered. Of course not everyone improves. I have already read the description of the interventions used in this study and will be adding a few of them to what I offer to see if this improves effectiveness.
I hope to launch an online education version of my Transforming Pain group in the new year. I will be watching the research literature for new developments. Sign up for my eNewsletter to be notified about upcoming courses and webinars.
A majority of participants becoming PAIN FREE after 4 weeks is something new in the field of persistent pain.
Author: Eleanor (Ellie) Stein MD FRCP(C)
I am a psychiatrist with a small private practice in Calgary and am an assistant clinical professor in the faculty of medicine at the University of Calgary. Since 2000, I have worked with over 1000 patients, all with ME/CFS, FM and ES. My passion for this field comes from my own struggle with these diseases, my desire to improve my health and then pass on what I learn. My goal is for every patient in Canada to have access to respectful, effective health care within the publicly funded system. If you are looking for help and resources to help combat ME/CFS, FM and ES, see my guides and webinar.
Want to Overcome Your Pain and Get Your Life Back?
Learn how to get rid of pain for good.
Healing Through Neuroplasticity Self-Study