Does Vitamin D Supplementation Lessen Chronic Pain?
Aug 14, 2025
How Do Our Bodies Make Vitamin D?
Vitamin D is actually a hormone rather than a vitamin. Like other hormones, vitamin D is made in the body, whereas vitamins are obtained through food. An inactive precursor of vitamin D is created in the skin on exposure to ultraviolet B radiation (290–315 nm) from sunlight.
Once formed in the skin, inactive vitamin D₃ (cholecalciferol) travels throughout the body. In the liver, it is transformed into 25-hydroxyvitamin D (25(OH)D), which is also inactive. This is the form of vitamin D we measure routinely in “vitamin D tests.” 25 (OH) vitamin D then travels to the kidneys, where it is further transformed to calcitriol (1,25(OH)₂D), the active form of vitamin D.
The active form of Vitamin D binds to vitamin D receptors (VDRs) found throughout the brain and body. Vitamin D regulates hundreds of genes (up to 10% of the human genome) related to immunity, cell growth, repair, and metabolism. In addition to maintaining healthy bones, calcitriol, the active form of vitamin D
- ensures enough calcium and phosphorus are absorbed from the diet and maintained at optimal levels,
- enhances both innate and adaptive immunity to protect us from infection, cancer and autoimmune conditions,
- supports healthy heart function, though we don’t know exactly how,
- regulates neurotransmitters, enhancing motivation and mood,
- decreases cancer risk and
- enhances insulin sensitivity.
Does Vitamin D Deficiency Cause Chronic Pain?
Research suggests a strong connection between chronic pain and lower vitamin D levels. The majority of studies are naturalistic population studies that compare people with “sufficient” 25-hydroxyvitamin D levels to those with “insufficient” levels. People with sufficient vitamin D levels are less likely to have chronic pain.
The cutoffs for deficient, insufficient and sufficient continue to be debated. The chart below is a consensus supported by many medical organizations, including the National Institute of Medicine and the Endocrine Society in the United States. The United States uses different units from the rest of the world. I have included the SI and American units so you can all check a recent vitamin D test result and see where you fall.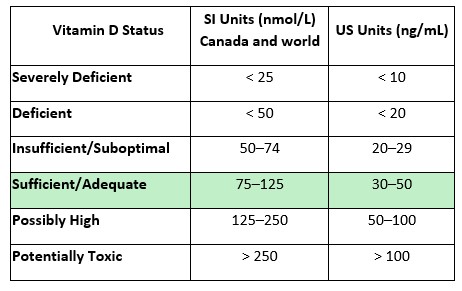
We don’t know exactly why low vitamin D is associated with chronic pain. It may be due to the impact it has on pain modulation and processing, including
- modulation of neurotransmitters known to be important for pain,
- the decrease in the release of inflammatory molecules, and
- the modulation of opioid receptors, which impact pain.
What Chronic Pain Conditions Are Associated With Vitamin D?
In a recent meta-analysis combining results from 81 observational studies with a total of 50,834 participants (Wu, Malihi, Stewart, Lawes, & Scragg, 2018), the majority of the studies (50 of the 81) found a correlation between lower vitamin D levels and the occurrence of chronic pain. Pain was more common in people with a vitamin D level below 50 nmol/L.
They found that, on average, people with arthritis, muscle pain and chronic widespread pain (including fibromyalgia) had lower levels of 25-hydroxy vitamin D than people without pain. And people with these types of chronic pain were about twice as likely to have vitamin D deficiency.
There was no correlation between vitamin D and headache pain, and it is unclear whether there is a correlation between vitamin D and other types of pain, such as neuropathic pain associated with diabetes and shingles.
A limitation of the Wu study is that it didn’t control for factors known to impact pain, such as lifestyle, socioeconomic status, and co-existing health conditions. And, believe it or not, when trying to find correlations between health variables in the general population, 50,000 people isn’t a large enough sample size to subgroup for all these interesting variables.
To address these weaknesses, a larger study was done using data from the UK Biobank, measuring the correlation between vitamin D levels and chronic musculoskeletal pain in 349,221 UK adults (Xie, Farrell, Armfield, & Sterling, 2024). They found that people with vitamin D levels below 50 nmol/L reported more chronic musculoskeletal pain than those with vitamin D levels ≥50 nmol/L. This finding persisted even after adjusting for variables that can impact both vitamin D levels and pain, such as age, sex, obesity, physical activity, and social and economic factors.
All this being said, the correlation between vitamin D and chronic pain was small. The people with lower vitamin D levels were 13% more likely to have chronic pain than those with higher levels.
Caution: Correlation Does not Mean Causation
Although this research may seem convincing—over 50 studies showing low vitamin D levels in people reporting painful conditions—just because two things occur together does not prove that one of the variables, e.g., low vitamin D causes the other, e.g., more pain. It could be, for example, that people experiencing chronic pain don’t get outside as much and have low vitamin D levels due to less exposure to UV light from the sun. It could also be that some other variable is decreasing pain levels, and vitamin D is a stand-in or biomarker for that other variable.
In Northern (and Southern) Latitudes, Vitamin D Insufficiency Is Common
Chronic pain is very common. Therefore, any dietary or lifestyle factor that contributes to chronic pain must also be common. Unfortunately, when it comes to vitamin D, this is the case. Data from the Canadian Multicentre Osteoporosis Study (CaMos) involving 1,912 participants from 7 cities showed that
- in the fall, 59% of Canadians have suboptimal vitamin D levels (<75 nmol/L).
- in the spring (after the winter in which there is little to no UVB light from the sun), 73.5% of men and 77.5% of women had levels <75 nmol/L.
- people with darker skin are more likely to have lower vitamin D levels because melanin blocks the absorption of ultraviolet light.
- people taking fortified dairy products or vitamin D supplements ≥400 IU/day were unlikely to be deficient.
How Much Vitamin D Should You Supplement?
I have been to dozens of conferences where the above statistics were presented, and the speakers concluded that everyone living above the 30th parallel (about where Atlanta, Georgia, is) should supplement with vitamin D to decrease inflammation and improve health.
This was the recommendation for a couple of decades. However, recent clinical trials of vitamin D supplementation in people with chronic diseases, including chronic pain, have found the evidence of benefit from supplementation to be inconclusive (Helde-Frankling & Björkhem-Bergman, 2017). Some studies show improvement with vitamin D supplementation in people with chronic pain, including fibromyalgia, and others do not.
Some studies suggest that people with insufficient or deficient vitamin D levels are more likely to benefit than those whose vitamin D is sufficient. This led Helde-Frankling and colleagues to suggest supplementation with 4000IU/day vitamin D for at least three months in people with vitamin D levels <30 nmol/L, with a goal of increasing the level to above 50 nmol/L.
The Endocrine Society (USA) updated its clinical practice guideline for vitamin D testing and supplementation in 2024. They suggest against routine testing of vitamin D levels. This means that many people won’t know their vitamin D levels. In Canada, it is very difficult to get a vitamin D test. The Endocrine Society doesn’t recommend routine supplementation, but does suggest the following groups may benefit irrespective of baseline vitamin D levels:
- children and adolescents aged 1 to 18 years to prevent nutritional rickets and because of its potential to lower the risk of respiratory tract infections due to the immune benefits of vitamin D;
- adults aged 75 years and older because of the potential to lower mortality due to infection and broken bones in people with osteoporosis;
- pregnant women because vitamin D decreases the risk of serious pregnancy and birth outcomes, including eclampsia and fetal death;
- people with high-risk prediabetes because vitamin D may reduce progression to diabetes.
The authors go on to state that, because there aren’t many food sources rich in vitamin D, supplementation should be obtained from fortified foods (milk and dairy products, for example) and vitamin D supplements. The Canadian Osteoporosis Society recommends supplementing with vitamin D in older adults. The website states, “The best way of getting vitamin D is through both food and supplements.”
Neither group mentions the safest and cheapest way to increase vitamin D levels—sunlight exposure.
Is Sun Exposure Beneficial?
Ultraviolet B (UVB) light activates the synthesis of vitamin D from cholesterol in the skin, causing all of the many benefits we have already discussed regarding vitamin D. But there’s more. Sunlight has many other beneficial effects not associated with vitamin D. The benefits of sunlight include
- modulating the immune system to be less reactive (↑Tregs);
- UVA ↑Nitric oxide. This lowers blood pressure and improves cardiovascular health.
- UVB ↑Beta-endorphin. This improves mood and reduces pain.
- bright light ↑serotonin. This improves mood.
- regulating circadian rhythm so that all the cells in the body work in sync with each other.
- infrared light (IR)↑ melatonin. This is the #1 antioxidant in the body and helps repair DNA damage from sunlight and decrease inflammation.
- IR ↑ mitochondrial function so the cells have enough energy to function optimally.
These cellular changes translate into significant, measurable health benefits, as reported by numerous researchers from various countries. Some of the benefits of sun exposure have been summarized by Hoel and colleagues (Hoel, Berwick, de Gruijl, & Holick, 2016). They include
- ↓ deaths from all causes (up to 15% fewer deaths by some modelling estimates)
- ↓ cases of and deaths from melanoma, colorectal, breast, prostate, and lymphoma cancers
- ↓ cardiovascular disease
- ↓ Alzheimer’s dementia
- ↓ multiple sclerosis, type I diabetes and other autoimmune diseases
- ↓ metabolic syndrome and type II diabetes
What Are the Risks of Sun Exposure?
Many people fear spending more time in the sun, believing it will increase their risk of skin cancer, particularly melanoma, which can spread and be fatal. It is true that sunburns double melanoma risk, especially when experienced in childhood. But non-burning, chronic sun exposure may be protective overall. Multiple studies have found that outdoor workers have lower rates of melanoma than indoor workers. This may be due to the increased production of melanin and melatonin when people are exposed to sunlight.
What Are the Dangers of Avoiding the Sun?
The public health warnings to stay out of the sun and wear sunscreen and sunglasses may be causing more harm than good. People who avoid the sun are 15% more likely to die from all causes. Hoel and colleagues make a case for what they call “safe sun exposure,” which is moderate, non-burning sun exposure sufficient to maintain vitamin D levels >75 nmol/L year-round. This can be achieved by exposing a large part of the body to the sun for 1 hour/day during the summer months. Because vitamin D is fat-soluble, it stays in the body for long periods.
So, you are less likely to die of metabolic syndrome, heart disease and cancer with more sun exposure, but will it help your pain?
Can Sunlight Reduce Pain?
An editorial in 2023 by Brzeszczyńska & Brzeszczyński summarizes some of the emerging treatments for chronic low back pain and concludes by suggesting that sunlight and melatonin (produced by sunlight) benefit pain at a far lower cost and less risk than experimental biomedical treatments.
Unfortunately, most research on light and chronic pain tests artificial light and not sunlight. A review of the impact of light on chronic pain on the website Physiopedia lists several studies of bright light therapy improving chronic pain, including fibromyalgia. Bright light is more beneficial when given in the morning, likely due to its impact on the body clock. There is growing research that red and infrared light benefits chronic pain and fibromyalgia, in particular (Yeh et al., 2019). And there is an intriguing study showing that exposure to green light for 8 hours daily for five days benefited people with fibromyalgia (Martin et al., 2021).
How Do You Know Whether Sunlight Has Any Benefits for You?
How could you figure out for yourself whether light will help your chronic pain? You could buy a large array of different-colored lights, or you could go outside more, including at least
- 10 minutes first thing in the morning,
- 1 hour at midday and
- another 10 minutes at dusk.
Sunlight contains bright light, UVB light, red and infrared light and green light. Whether purposefully increased sunlight exposure benefits chronic pain deserves research. Since one cannot patent or sell sunlight, no companies are motivated to fund research on sunlight.
I recommend doing your own “n of 1” study. Record what your pain levels are now and the ways in which pain interferes with your life. Then create your own “treatment” plan, getting outside consistently, something you can sustain over the long term, and observe whether it benefits you or not. Then let me know!
To see the Video Tip corresponding to this blog, click here.
If you liked this blog, you may also like the following similar blogs:
https://www.eleanorsteinmd.ca/blog/does-magnesium-improve-sleep
https://www.eleanorsteinmd.ca/blog/hydrogen
https://www.eleanorsteinmd.ca/blog/magnesium
https://www.eleanorsteinmd.ca/blog/new-information-on-calcium-supplementation
To learn more about Live! with Dr. Stein, click the image below. 
References:
Helde-Frankling, M., & Björkhem-Bergman, L. (2017). Vitamin D in Pain Management. Int J Mol Sci, 18(10). doi:10.3390/ijms18102170
Hoel, D. G., Berwick, M., de Gruijl, F. R., & Holick, M. F. (2016). The risks and benefits of sun exposure 2016. Dermato-endocrinology, 8(1), e1248325. doi:10.1080/19381980.2016.1248325
Martin, L., Porreca, F., Mata, E. I., Salloum, M., Goel, V., Gunnala, P., . . . Ibrahim, M. M. (2021). Green Light Exposure Improves Pain and Quality of Life in Fibromyalgia Patients: A Preliminary One-Way Crossover Clinical Trial. Pain Med, 22(1), 118–130. doi:10.1093/pm/pnaa329
Wu, Z., Malihi, Z., Stewart, A. W., Lawes, C. M., & Scragg, R. (2018). The association between vitamin D concentration and pain: a systematic review and meta-analysis. Public Health Nutr, 21(11), 2022–2037. doi:10.1017/s1368980018000551
Xie, Y., Farrell, S. F., Armfield, N., & Sterling, M. (2024). Serum Vitamin D and Chronic Musculoskeletal Pain: A Cross-Sectional Study of 349,221 Adults in the UK. J Pain, 25(9), 104557. doi:10.1016/j.jpain.2024.104557
Yeh, S. W., Hong, C. H., Shih, M. C., Tam, K. W., Huang, Y. H., & Kuan, Y. C. (2019). Low-Level Laser Therapy for Fibromyalgia: A Systematic Review and Meta-Analysis. Pain Physician, 22(3), 241–254. doi:10.36076/ppj/2019.22.241

